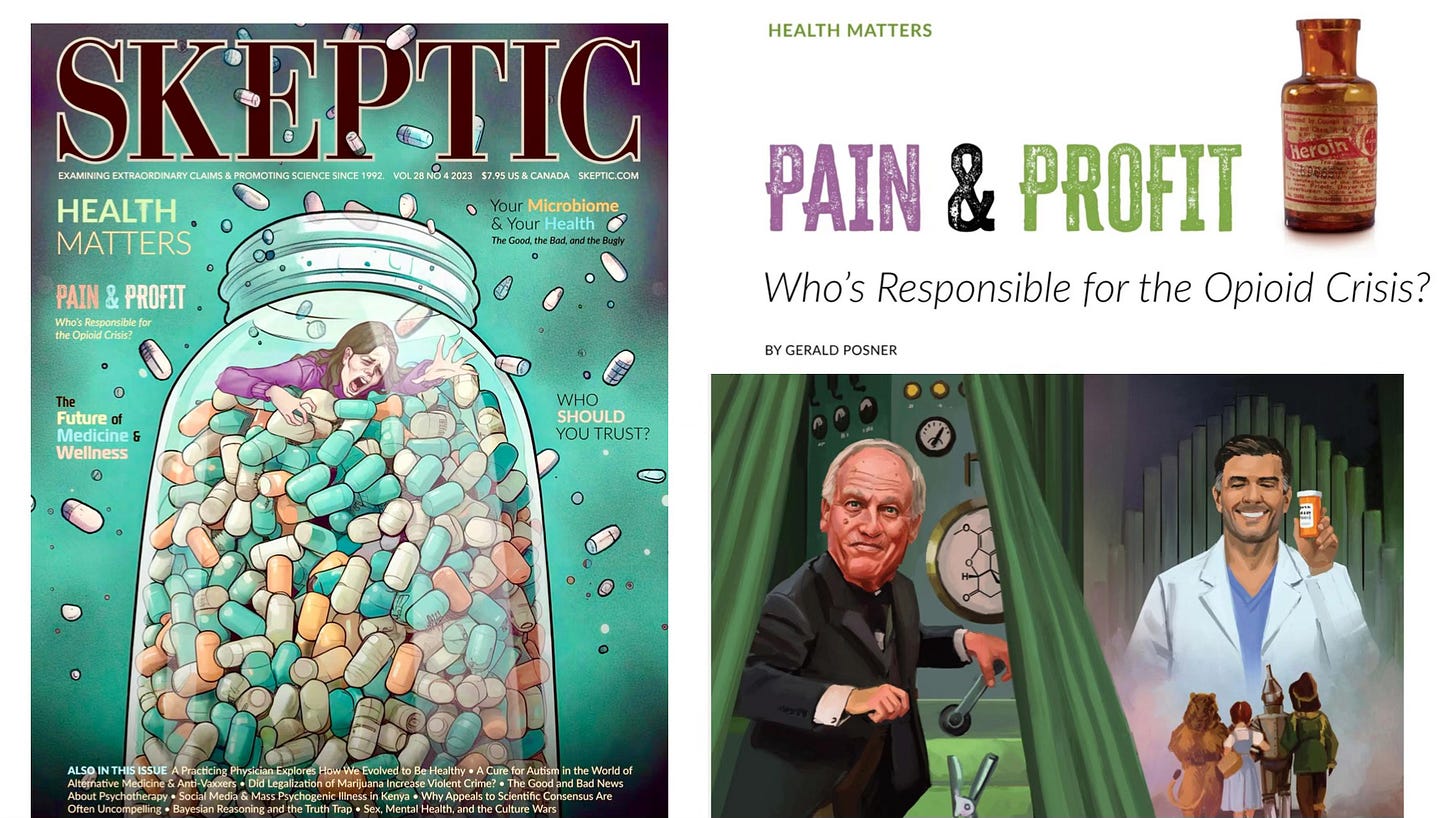
Pain and Profit
Who is Responsible for the Opioid Crisis?
The following is a reprint of my article - “Pain and Profit: Who Is Responsible for the Opioid Crisis” - in the previous issue of Skeptic magazine. Thanks to Michael Shermer for giving me the green light to share this with my Just the Facts subscribers. (Please note, this is a long form article. If this newsletter is truncated in your email, just click “View the entire message” and you can read the full piece.)
In 2021 the CDC issued a grim statistic: more than one million Americans had died from overdoses since 1999 when it started tracking an opioid epidemic that began with prescription painkillers and is now dominated by fentanyl.[i] Since that sobering milestone another 300,000 have died.[ii] That is roughly the same number of Americans who died in all wars the United States has entered (1.3 million) combined, including the First and Second World Wars and the Civil War.[iii] The opioid epidemic is, aside possibly from obesity, the biggest health crisis of our time.
Most know about the frenzy of f…